Although Schmorl’s nodes in the past have been considered clinically insignificant, clearly they can be an active symptom or cause of pain in some patients.
The Schmorl’s Node Controversy
Schmorl’s nodes refer to protrusions of intervertebral disc cartilage through the vertebral body endplate and into the adjacent vertebra. (Figure 1.) Lateral herniations that impinge spinal roots are more commonly expected. But Schmorl’s node herniations are vertical.
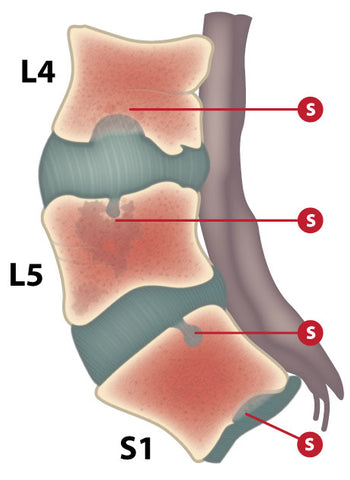
Figure 1. Schmorl’s nodes (S)
These vertebral herniations, named after German pathologist Christian Georg Schmorl (1861–1932)—also called intravertebral disc herniations or Schmorl nodes—are distinguished from bone infection and malignancy. However, comorbidities should not be overlooked.
Hypothetically, a patient with a history of Schmorl’s nodes could contract an infection that leads to vertebral osteomyelitis. Disc herniation may also be complicated by unrelated tumor growth.
Protrusions can contact the marrow of the vertebra, possibly leading to inflammation or remaining asymptomatic. The protrusions are also associated with necrosis of the vertebral bone. Whether this prolapse and inflammation cause the necrosis, or whether the cartilage migrates into areas that have become necrotic due to other conditions, is under investigation.
Forces normally distributed by the nucleus pulposus (the incompressible gelatinous center of the intervertebral disc) are concentrated in a certain area causing endplates to deform in a concave manner.
Initial Identification
Although Schmorl’s nodes in the past have been considered clinically insignificant, clearly they can be an active symptom or cause of pain in some patients. T.R. Yochum states that Schmorl’s nodes may be caused by numerous factors: trauma; hyperparathyroidism; osteoporosis; Schuermann’s disease; osteomalacia; infections; and neoplasm.
According to pathogenesis of 12 surgical specimens by B. Peng, vertebral marrow cavities (less often seen in X-rays) are not empty, but an ingrowth of fibrous tissue or fibrocartilage from the necrotic area into the cartilaginous endplate.
The hypotheses of Schmorl’s nodes origin and pathogenesis include developmental factors, degenerative conditions, pathological processes such as infection, neoplasia, and trauma.
Studies have demonstrated that nucleus pulposis activates the release of inflammatory hormones and enzymes (such as leukotrenes, cytokines, PLA2, substance P, etc.), and as such may be responsible for C-nociception or diffuse vertebrogenic pain. Peng suggests that Schmorl’s nodes are the result of ischaemic necrosis beneath the cartilaginous endplate and that herniation into the body of the vertebra is secondary.
Does It Hurt?
In symptomatic patients, the vertebral body marrow surrounding Schmorl’s node gives a low signal intensity on T1-weighted and a high signal intensity on T2-weighted images. This indicates the presence of inflammation and edema within the vertebral bone marrow. These MRI findings were not present in asymptomatic individuals which suggested that Schmorl’s nodes became asymptomatic when the inflammation subsided.

Figure 2. Schmorl’s nodes evident in MRI.
F.M.K. Williams and colleagues note that Schmorl’s nodes etiological significance for back pain may be due to lumbar disc disease, as the two commonly occur simultaneously. N.S.M. Neves, et al. reports significantly decreased pain following percutaneous biopsy revealing fibrocartilaginous fragments, similar to the intervertebral disc, with no signs of a malignant or infectious process. Schmorl’s nodes are better identified on CT images, and best seen on MRI. (Figure 2.)
Acute herniation can appear more aggressive with surrounding bone marrow edema and peripheral enhancement. If pain is present, it can last a few years before subsiding.
There is a case reported by Seon Joo Park, Ph.D, et al. of complete separation of a vertebral body caused by an untreated Schmorl node accompanying severe osteoporosis. Active herniation can increase the risk of vertebral fractures by about 10 percent. Orthopedics doctors may recommend vertebroplasty as an effective remedy, especially when fractures are combined with osteoporosis.
To support the writing of scholarly articles about orthopedics, ClinicalPosters sells human anatomy charts, scientific posters, and other products online. You may sponsor specific articles or remit a small donation.
ClinicalPosters sells human anatomy charts, scientific posters, and other products online to offset expense of the writing useful articles about orthopedics. Slide extra posters into DeuPair Frames without removing from the wall.
Show your support by donating, shopping for ClinicalPins, or leaving an encouraging comment to keep the research going.
To support the writing of useful articles about orthopedics, ClinicalPosters sells human anatomy charts, scientific posters, and other products online. You may sponsor specific articles or remit a small donation.
ClinicalPosters sells human anatomy charts, scientific posters, and other products online to offset expense of the writing useful articles about orthopedics. Slide extra posters into DeuPair Frames without removing from the wall.
ClinicalPosters sells human anatomy charts, scientific posters, and other products online. You may remit a small donation.
You can support the writing of useful articles about orthopedics by sponsoring specific articles or remitting a small donation. Visible content is optimized for device size.






 Romance & Health Intertwine. Fall in love with a captivating romance miniseries that explores the essence of well-being. Become a ClinicalNovellas member for heartwarming tales.
Romance & Health Intertwine. Fall in love with a captivating romance miniseries that explores the essence of well-being. Become a ClinicalNovellas member for heartwarming tales.




