Instead of a speedy confirmation, I had multiple diagnoses amid diminishing confidence in my medical team.
Follow My Lump-Diagnosis Saga
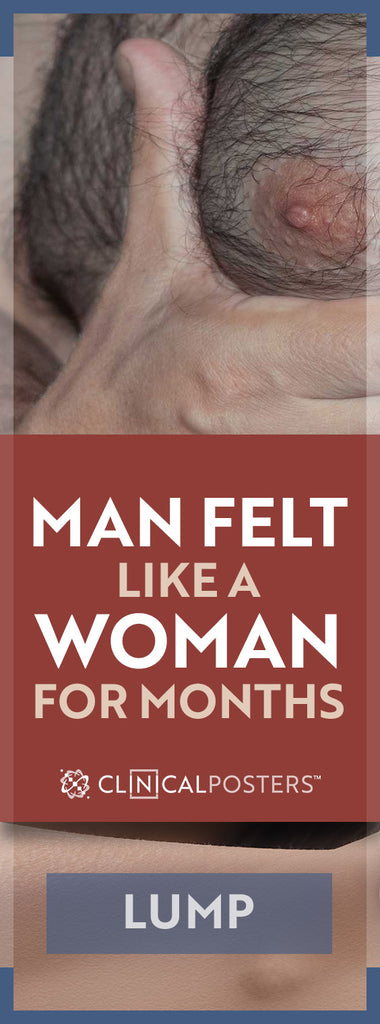
While toweling off after a shower, something seemed anatomically amiss. I paused and wondered why it felt like my nipple was under my arm. Is my flesh that pliable or is this a newfound growth? Wiping the fog from the mirror, and raising an elbow, revealed nothing out of place.
With circular motions, I began my breast self-examination (BSE). After confirming a palpable lump, I did what most people do when plagued with health questions—search the Internet. There, as you might expect, I learned the course of wisdom is to schedule a doctor’s appointment for an evaluation if it does not resolve within three weeks.
Based upon further research, in the months that followed, A Bit More Healthy blog was filled with useful advice for various outcomes—mostly so I could better understand the process and make pertinent inquiries during consultations. It also coincided with health awareness months.
In hindsight, a diagnosis could have been confirmed more efficiently within one month. At the end of this story, we will prune out unnecessary steps to make your journey more productive, should you find yourself in a similar situation. Pour yourself a hot beverage and read on.
Empirical Evaluation
Patient Story: It took three weeks for my scheduled appointment with a primary care provider (PCP). This coincided with my annual physical exam. Palpating the area of concern, he suspected a lipoma because the subcutaneous mass was moderately firm and somewhat mobile. Eight different categories of lipoma differ in composition and density.
To rule out inflammation, my doctor prescribed a 10-day antibiotic that made me ill for the first few. In two weeks, both my lump and I returned to the doctor. With the preliminary non-life-threatening lipoma diagnosis, barring cosmetic considerations, excision is not generally required. However, location and family history can indicate a more cautious approach. I looked forward to the ultrasound the following week with prudent and cautious optimism.
Thinking about the irony of ultrasounds for a pregnant woman, my wit was wasted on the radiologist when I quipped, “I hope you don’t find twins” (referring to multiple lumps). If you have seen the now canceled show, ‘Til Death, season 1, episode 6, or ever tried to pry a diagnosis from a medical technician, you realize how difficult it is to gather useful information. Nevertheless, I pressed further, questioning the capability of the equipment.
“Are you able to distinguish a lipoma using ultrasound?” He said it was possible. After several image grabs, he called in a second radiologist. She rubbed the wand over the same area, confirmed the diameter with the original radiologist and exited. Wiping away the gel, I remarked, “Double checking is good.” I was excused with no indication of diagnosis, fully expecting a validating report would soon follow.
There’s a Problem
Weeks went by while my PCP was out of the office. Generally, I communicate with my doctors via secure email through an approved hospital portal. Hence, the person-to-person phone call I received heightened concern over the results. I was told that the ultrasound was inconclusive. There was an authoritative urgent recommendation for an MRI.
Optimism can morph into anxiety in the absence of affirmation. But I strived to maintain composure while continuing my regular activities. Another week passed before the MRI was performed. I asked the technician for a peek as a frame of reference. Another patient was already queued up in the chamber when I got dressed.
Apprehensively, the technician flipped though my images in a small window on a computer screen, flip-book style in about 6 seconds. That was a useless quick peek.
Since my PCP was out of the office again, it took over a week before I received the shocking lab results via email. They could not locate the mass! I’m perplexed. Now it’s gone? Time for another BSE. I literally felt (my breast) like a woman. “Lump is still there.”
Questioning my doctor about the report caused him to respond with another explanation: “It could be inflammation.” Wait, wasn’t that what the antibiotic was for? So instead of a speedy confirmation, I had multiple diagnoses, amid diminishing confidence in my medical team.
At this point I requested a second opinion. My PCP promptly replied that he would arrange for a surgeon within the health network to review the MRI with me. About 10 days later I was viewing some of the most pathetic MRI images I have ever seen. Not only was the area in question only tangentially included, the fidelity was fuzzy—apparently imaged with low-Tesla, or improperly maintained equipment. It was virtually useless. The ultrasound that depicted a faint 1.7 cm mass was all we had to go on.
Did You Say, “Cancer?”
Surgeons have an interesting profession. They like to cut people open. During my surgical consult, two surgeons weighed the pros and cons of an excisional biopsy. Pro: Remove the mass and end the mystery. Con: If it turns out to be cancerous, there would be a need to remove more tissue and accurate post-op imaging would be difficult because of the initial biopsy and swelling.
OK, now they went there. That’s the “C” word. Stay calm. Logic was sound. However, the next words stripped me of any remaining masculinity.
Protocol is mammography. You’re kidding, right? Squeezing my “breast” between two hands, I asked, “Is it even possible for men?” I was told that some women with less tissue are able to receive mammograms. Should I feel buffed or like I have gynecomastia? A male oncology surgeon, a physician’s assistant and a nurse, were all seriously staring at me for a response. I said, “OK, I'll consent to mammography.”
The following week, I encountered a fear common among women; some call it a breast panini press or vise grips. Others say it’s like squeezing a breast in a refrigerator door. Despite the horror stories and glares from women in the pink waiting room, I was endeavoring to man up for a male mammogram.
How did it really feel? The procedure for two views was relatively quick, resembling a firm but dull pinch. The doctor said that he found nothing out of the ordinary.
How Many Diagnoses?
Over two months had gone by and I was no closer to confirmation of a diagnosis. Now the surgeon who ordered the mammogram was out of town. This delayed my official pathology report and follow-up visit. In her absence, my PCP forwarded to me the results stating that it was a “benign” lymph node.
The doctor apparently used quotes because it’s common knowledge that biopsy is the only definitive way to come to such a conclusion. At this point, it is sobering to review the things I have been told thus far:
- It’s probably a lipoma.
- It’s a suspicious unidentified mass.
- It vanished.
- It could be inflammation.
- Let’s cut it out to see if it’s cancer.
- It’s nothing abnormal.
- It’s a “benign” lymph node.
Should subtle tonality on the initial ultrasound have signaled subsequent radiologists to tune exposure for lower contrast? Apparently, the technicians used default settings. Empirically, the “disappearance” on film and faint ultrasound had me suspecting the mass was of similar substance as surrounding tissue, hence a lipoma.
I couldn’t seem to get two professionals to agree on anything. Another two weeks again found me face to face with Dr. Cuts. Actually, she is quite kind and calmly addressed my concerns. “So are we going to remove a lymph node?” I asked. Filled with questions, I further inquired, “Since a lab only performs tests ordered by the physician, shouldn’t I see an endocrinologist or oncologist who specializes in lymphoma?” “A specialist might order specific tests that a general surgeon might not think of. Once the mass has been removed, won’t this prevent subsequent tests from being performed?”
She replied that though located in the same general vicinity, she had doubts about it being a lymph node. I was assured that the pathologist would be thorough—even enlisting an outside lab if necessary. The recommended course of action is excisional biopsy. Having already paid for this second visit with her and exhausted non-invasive options, I consented to a subcutaneous left chest/flank excisional biopsy.
Under the Knife
Lying on my side with arm raised, the area was sterilized. In my position I could not view what was happening. There was a noticeable prick from the first injection of local anesthetic. Several more followed. While we carried on a dialogue, unbeknown to me, the shots morphed into an incision. The surgical procedure was seamlessly underway.
Concerned over the amount of bleeding, the surgeon asked her assistant to prepare a cauterizing knife that sears off blood vessels while cutting. A patch was grounded to my leg to prevent electric shock. After a few more minutes of cutting, I heard, “Here it is,” showing me a nodule about the size of a peanut. “It looks like a lipoma but we’ll send it to the lab to confirm. You should hear back before the week is over.” It resembled the self-limiting lipomas I saw on the Web so I was a bit relieved.

Medical offices frequently use 3M™ Kind Removal brand of tape with gauze. A dissolvable “glue” type “bandage” that lasts a few days was applied over the dissolvable stitches. This technique keeps the wound dry even when showering. Completely awake during the entire procedure, I felt no pain. When the surgeon was done, I walked out unassisted and drove home.
Paying two bucks to the parking attendant meant I was there under an hour. About six hours later, the local anesthetic subsided. It now felt like I had been scratched or pricked—no real pain though—more on par with an itch. A single OTC ibuprofen subdued the annoyance.
Pathology Report
Two days later, as originally suspected, a benign lipoma was confirmed. Good news: there are no cancer cells in the mass. Essentially, it’s just a piece of dense fat. Had the ultrasound technician confirmed this, it could have saved weeks of apprehension and 90 percent of the total doctor bill.
Involving a specialist early on may have prevented much of the unnecessary testing while (s)he focused on the suspected diagnosis. This opportunity to walk in a woman’s shoes without wearing stilettos has given me more compassion for the things ladies go through to keep breasts healthy.







 Romance & Health Intertwine. Fall in love with a captivating romance miniseries that explores the essence of well-being. Become a ClinicalNovellas library member for heartwarming tales.
Romance & Health Intertwine. Fall in love with a captivating romance miniseries that explores the essence of well-being. Become a ClinicalNovellas library member for heartwarming tales.




