There is no specific blood test for lymphoma.
Seriousness of Blood Cancer
Leukemia & Lymphoma Awareness month goes beyond wearing a colored ribbon or taping a flyer in a clinic window. Doctors should be attuned to differentials and patients must voice concerns over unexplained symptoms—perhaps insisting on accurate testing rather than empirical evaluations.
Lymphoma is a cancer of the lymphocytes (white blood cells) that typically play a key role in fighting infection. The lymphatic system is part of the circulatory system, comprising a network of conduits called lymphatic vessels that carry a clear fluid called lymph towards the heart. Collections of lymph nodes are found in the neck, underarms, chest, abdomen, and groin.
Lymphatic tissue is also located in other parts of the body, including the stomach, skin, and small intestine. Beyond oncology, a multidisciplinary approach enlisting experts in cardiology, dermatology, rheumatology, neurology, immunology, and vision care is useful to optimally manage patients with rare or complex neoplasms.
There are two broad types of lymphoma—Hodgkin lymphoma (HL) or non-Hodgkin lymphoma (NHL) and many subclassifications. The main difference between HL and NHL is in the specific lymphocyte each involves. Because of so many variations, it is not uncommon for medical practitioners to offer differing diagnoses for the same symptoms or even lab results.
In fact, a second opinion of pathologist biopsy interpretation (whether negative or positive) may be equally, if not more, important than a second opinion for an oncologist’s treatment plan. Differences between malignant and benign cells can be subtle and interpretations can be subjective.
People with Sjogren’s syndrome are 44 times more likely to develop non-Hodgkin lymphoma.
With about 66,000 cases diagnosed each year, non-Hodgkin lymphoma (NHL) can cause many different signs and symptoms, depending on where it is within the body. In some cases NHL might not cause any symptoms until it grows quite large. If any of the following symptoms persist for more than a few days, seek medical evaluation [1]:
The Eyes Have It
Dry eyes and aching joints can be precursors to lymphoma since people with Sjogren’s syndrome are 44 times more likely to develop NHL. If you have Sjogren’s syndrome, report any of the main early NHL symptoms to your general practitioner—a painless swelling in a lymph node (gland), usually in the neck, armpit or groin.
Mucosa-Associated Lymphoid Tissue (MALT) lymphoma affects lymphatic tissue in parts of the body such as the stomach, gut, lungs, and eyes. This B-cell lymphoma can, therefore, manifest dry eyes as a secondary symptom.
B-Cell Lymphomas
In the United States, B-cell lymphomas (lymphocytes originating from bone marrow) account for about 85% of non-Hodgkin lymphomas. The most common type is diffuse large B‑cell lymphoma (DLBCL) with an average onset of 63-66 years of age. It is distinguished as a quickly growing mass within a lymph node.
Therapeutic targets for diffuse large B‑cell lymphoma include RelA NF-κB and IRAK4 Kinase.
Primary mediastinal B-cell lymphoma (PMBCL) accounts for only 2% of all lymphomas. It is more prevalent among women in their 30s. PMBCL is similar to DLBCL but with fibrosis and generally localized in the middle of the chest. Both types respond well to treatment. Intravascular large B‑cell lymphoma is a rare subtype of DLBCL affecting blood vessels.
Follicular lymphoma has nothing to do with the skin or hair shaft. It describes slow-growing cells that form a circular pattern within lymph nodes. References provide details for additional less-common B‑cell lymphomas listed below. [2]
- Chronic lymphocytic leukemia /small lymphocytic lymphoma
- Mantle cell lymphoma
- Marginal zone B-cell lymphomas
- Burkitt lymphoma
- Lymphoplasmacytic lymphoma
- Hairy cell leukemia
- Primary central nervous system (CNS) lymphoma
T-Cell Lymphomas
More rare T-cell lymphomas (lymphocytes originating from thymus) make up the remaining 15% of non-Hodgkin lymphomas in the United States. Precursor T-lymphoblastic lymphoma can be considered a leukemia as more bone marrow involvement increases. Since this disease often originates in the thymus, breathing, and cardiovascular impediments may develop. [2]
Peripheral T-cell lymphomas have many subcategories:
- Cutaneous T-cell lymphomas (CTCL)
- Angioimmunoblastic T-cell lymphoma
- Extranodal natural killer/T-cell lymphoma, nasal type
- Enteropathy type intestinal T-cell lymphoma
- Anaplastic large cell lymphoma (ALCL)
- Unspecified peripheral T-cell lymphoma
Largest Organ in Lymphatic System is the Skin
Though most lymphomas manifest within internal organs, cutaneous T‑cell lymphomas (skin lymphoma or mycosis fungoides) can be observed externally. The problem with diagnosis is that there is great variation in appearance.
Cutaneous pseudolymphoma is not a disease but rather an inflammatory response to known or unknown stimuli that results in a lymphomatous-appearing but benign accumulation of inflammatory cells.
Pseudolymphomas often show broad patches and plaques. They often mimic cutaneous T-cell lymphoma. Examples include actinic reticuloid, lymphomatoid contact dermatitis, and lymphomatoid drug eruptions.
Mycosis fungoides (MF) makes up 72% of CTCL. Sezary syndrome is an advanced, variant form of MF, which is characterized by the presence of lymphoma cells in the blood. Extensive thin, red, itchy rashes usually cover over 80% of the body in MF.
CTCL typically presents with red, scaly patches or thickened plaques of skin that often mimic eczema or chronic dermatitis. They are generally treatable but not curable. Mycosis fungoides (no relation to fungus) initially consist of flat, pink lesions which may be oval or annular, and may be accompanied by itching and thinning of the skin.
Lesions thicken and itch more in the plaque stage. The tumor stage sees the development of large, possibly ulcerated irregularly shaped lumps on plaques. Cutaneous B‑cell lymphomas (CBCL) are a less common version of cutaneous lymphomas, making up about 20-25% of all cutaneous lymphomas. [3,4]
After growing for several years, cutaneous lymphoma may become systemic and manifest itself within lymph nodes. Early diagnosis and treatment are indicated for a favorable prognosis. In Practical Dermatology, Lawrence A. Mark, MD, PhD shares his method of early mycosis fungoides identification. Excerpts below:
Classic MF primarily arises in the double-clothed areas of the body: axillae, breasts, groin, and buttock primarily presented with thin, red, scaly, poorly demarcated plaques of at least 5cm in diameter. Over time the morphology tends toward thickening of the plaques to more erythematous prominence, and, of course, tumors that may ulcerate.
Early MF can be subtle and usually lacks classic histopathologic signs, thereby causing so much trouble in making the early definitive diagnosis. This is why I do not rely solely on pathology to confirm early-stage disease.
Classic histopathology of MF reveals all of the following: lichenoid dermatitis with “Indian file” lining up of atypical lymphocytes at the dermo-epidermal junction, exocytosis of atypical lymphocytes, minimal or no spongiosis, wiry collagen in the papillary dermis, and Pautrier’s microabcesses (which are nearly pathognomonic). Having a few of these histologic features present is variably suggestive of MF, depending on which ones and how many are present. [5]
Lymphoma Outlook and Prognosis
Slow-growing lymphomas have the best early cure rate. The dichotomy is that they are generally discovered after the disease has progressed to an advanced stage. High-grade aggressive lymphomas are often symptomatic early on and are potentially curable with aggressive treatments.
Because the lymphatic system extends to so many parts of the body, it may first be suspected by dermatologists, cardiologists, gastroenterologists, pulmonologist, internists, neurologists or during ob-gyn examinations. There is no specific blood test for lymphoma.
Pathologists or hematologists can only observe irregularities in blood counts. Similarly, radiology scans are useful in detecting abnormal masses but cannot distinguish between benign and malignant tumors. A constellation of tests and symptoms narrow down a diagnosis. Flow Cytometry has advanced over the past decade to a useful tool in detecting lymphoma. [6]
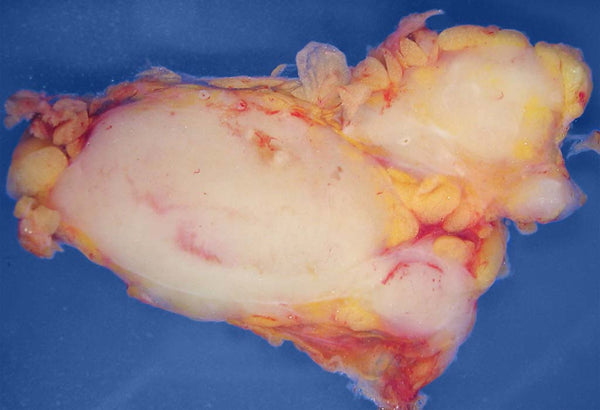
Macroscopic aspect of the cut surface of a human lymph node replaced by lymphoma. The node is about 6 x 4 cm (2.5" x 1.5"). The nodules of pinkish-white tissue surrounded by yellowish fatty tissue represent lymphoma. Histological examination revealed follicular lymphoma. [7]
Pain is not a primary symptom. Skin lesions that do not heal, deep or surface lumps in the neck, armpits, chest, breasts, abdomen, or groin should be brought to the attention of appropriate medical professionals. Diagnosis may involve a physical exam, blood tests, imaging tests, and/or surgical biopsy of a swollen lymph node or bone marrow collection to determine the A or B category of four progressive stages. [8]
It is estimated that 9,290 men and women (5,070 men and 4,220 women) were diagnosed with Hodgkin’s lymphoma in 2013. [9] According to the American Cancer Society, about 74,680 people, including children, (41,730 males and 32,950 females) will be diagnosed with NHL this year.
Lymphomas can migrate from one type to another (i.e. skin to lymph node) so follow-up examinations are important. Nevertheless, try not to panic if symptoms are discovered. Lymphomas are statistically less likely to occur than more benign differentials such as lipomas or eczema. In 2009, The National Institute of Health designed and established a multidisciplinary cutaneous lymphoma clinic (MCLC) at the Ohio State University. [10]
Underarm Darkening
Acanthosis nigricans (AN) can cause thickening of the skin or darkening in other areas of the body, such as the neck, underarms, and groin. It has a prevalence according to age, race, and body weight. In rare cases, AN can also occur because a cancerous tumor is growing in the stomach, liver, or another internal organ. This form of AN is called malignant acanthosis nigricans. [11]
To remain A Bit More Healthy, unusual symptoms should be professionally evaluated, particularly during September Leukemia and Lymphoma Awareness Month. See references for questions you can ask your doctor about non-Hodgkin Lymphoma [12] and for the best U.S. hospitals with oncology departments. [13]
To support the writing of scholarly articles about oncology, ClinicalPosters sells human anatomy charts, scientific posters, and other products online. You may sponsor specific articles or remit a small donation.
ClinicalPosters sells human anatomy charts, scientific posters, and other products online to offset expense of the writing useful articles about oncology. Slide extra posters into DeuPair Frames without removing from the wall.
Show your support by donating, shopping for ClinicalPins, or leaving an encouraging comment to keep the research going.
To support the writing of useful articles about oncology, ClinicalPosters sells human anatomy charts, scientific posters, and other products online. You may sponsor specific articles or remit a small donation.
ClinicalPosters sells human anatomy charts, scientific posters, and other products online to offset expense of the writing useful articles about oncology. Slide extra posters into DeuPair Frames without removing from the wall.
ClinicalPosters sells human anatomy charts, scientific posters, and other products online. You may remit a small donation.
You can support the writing of useful articles about oncology by sponsoring specific articles or remitting a small donation. Visible content is optimized for device size.






 Romance & Health Intertwine. Fall in love with a captivating romance miniseries that explores the essence of well-being. Become a ClinicalNovellas library member for heartwarming tales.
Romance & Health Intertwine. Fall in love with a captivating romance miniseries that explores the essence of well-being. Become a ClinicalNovellas library member for heartwarming tales.




